Table of Contents
Introduction
In the intricate tapestry of global health, there exists a threat as old as time yet as present as the air we breathe—dengue disease. Often cloaked in the guise of a mere fever, its reach extends far beyond a simple ailment, affecting millions with its virulent touch. As a doctor, I’ve witnessed the stealthy advance of this disease and the profound impact it has on lives. This article isn’t just a collection of facts; it’s a beacon of knowledge, a shield against an invisible enemy. So, I invite you to join me on a journey of discovery, to unravel the mysteries of dengue disease, and to arm yourself with the power of awareness.
What is Dengue?
Dengue is not just a disease; it’s a global phenomenon caused by a virus (Flavivirus) transmitted through the bite of an infected Aedes mosquito. It’s a chameleon of sickness, presenting itself through a spectrum of symptoms that can range from a mild fever to severe, life-threatening conditions. The dengue virus comes in four different serotypes, each capable of painting a unique clinical picture. When the mosquito’s proboscis pierces the skin, the virus enters the bloodstream, setting the stage for a battle between the invader and the body’s defenses.
Causes of Dengue Disease
Dengue fever is caused by one of four closely related dengue viruses. These viruses are transmitted to humans through the bite of an infected Aedes mosquito, primarily Aedes aegypti and to a lesser extent Aedes albopictus. These mosquitoes are tropical and subtropical creatures that thrive in and around human lodgings. They breed in stagnant water that can collect in artificial containers, making urban environments ripe for their proliferation.
Key Points to Understand:
- Transmission: The dengue virus is not contagious and cannot spread directly from person to person. Instead, it is transmitted through mosquito bites1.
- Mosquito Breeding: Common breeding grounds include standing water in buckets, bowls, animal dishes, flower pots, and vases1.
- Global Spread: While dengue is most prevalent in tropical and subtropical climates, global travel and trade have facilitated its spread to new areas2.
- Multiple Strains: There are four different dengue virus serotypes (DENV 1-4), and infection with one type usually gives lifelong immunity to that type, but only short-term protection against the others.
- Second Infection Risk: Subsequent infections by different serotypes increase the risk of developing severe dengue
Signs and Symptoms of Dengue Fever

Dengue disease is a mosquito-borne illness that can range from mild to severe. The onset of symptoms typically begins 4-10 days after being bitten by an infected mosquito, and these symptoms usually last for 2-7 days. Here’s what individuals should be aware of:
- High Fever: A sudden, high fever that can reach up to 40°C/104°F is often the first sign of dengue.
- Severe Headache: Intense headache, often described as being located behind the eyes. Read about migraine headaches here.
- Muscle and Joint Pains: Widespread pain in muscles and joints, sometimes severe enough to be incapacitating.
- Nausea and Vomiting: Gastrointestinal symptoms such as nausea and vomiting may occur.
- Rash: A skin rash that appears two to five days after the onset of fever.
- Mild Bleeding: Such as a nose or gum bleed, easy bruising, or blood spots under the skin.
Severe Dengue Fever Symptoms
In a small percentage of cases, the disease can progress to severe dengue, also known as dengue hemorrhagic fever, which can be life-threatening. Symptoms of severe dengue include:
- Abdominal Pain: Intense and continuous pain in the abdomen.
- Persistent Vomiting: Vomiting that doesn’t stop can lead to severe dehydration.
- Rapid Breathing: Difficulty breathing or fast breathing.
- Bleeding: More severe bleeding than with mild dengue, such as from the gastrointestinal tract.
- Fatigue and Restlessness: Feeling unusually tired, restless, or irritable.
Remember, while dengue can be a serious illness, early detection and proper medical care can significantly reduce the risks of complications. It’s important to stay informed and take preventive measures to protect yourself and your community from dengue fever.
Clinical Diagnosis

Dengue disease can present symptoms similar to other diseases like chikungunya, Zika virus, malaria, and typhoid fever, which can make clinical diagnosis challenging. Healthcare providers will consider dengue in patients with acute onset of fever, headache, body aches, and sometimes a rash, particularly if they live in or have recently traveled to a dengue-endemic area.
Laboratory Diagnosis Laboratory tests are essential to confirm a dengue diagnosis:
- Nucleic Acid Amplification Tests (NAATs): These tests, including reverse transcription-polymerase chain reaction (rRT-PCR), are preferred for patients suspected of having dengue virus disease. They should be performed on serum specimens collected within 7 days after symptom onset. The presence of viral genomic sequences or dengue nonstructural protein 1 (NS1) antigen in a single diagnostic specimen is considered confirmation of dengue.
- Serologic Tests: IgM antibody testing can identify additional infections and is an important diagnostic tool. However, interpreting the results can be complicated by cross-reactivity with other flaviviruses. IgM against dengue virus can be detected with MAC-ELISA, usually 4 days or more after fever onset. For patients presenting during the first week after fever onset, diagnostic testing should include a test for dengue virus (rRT-PCR or NS1) and IgM. For patients presenting more than a week after fever onset, IgM detection is most useful.
- Plaque Reduction Neutralization Test (PRNT): This test can resolve false-positive IgM antibody results caused by non-specific reactivity and, in some cases, help identify the infecting virus. It’s considered the gold standard for dengue serology.
Points to Remember
- Dengue is a nationally notifiable disease in many countries, so all suspected cases should be reported to local health departments.
- Early diagnosis and proper management are key to reducing the risk of complications.
- Patients should receive appropriate management to monitor for shock and complications resulting from increased vascular permeability and plasma leakage without waiting for diagnostic test results.
Blood Test A blood sample is taken to look for signs of the dengue virus or antibodies to it. This test may also identify which of the four dengue virus serotypes is causing the infection.
Awareness for Individuals
- If you become sick after traveling to a tropical area, inform your healthcare provider.
- Early reporting of symptoms and travel history can greatly aid in the timely diagnosis of dengue.
By understanding the diagnostic process for dengue fever, healthcare professionals can ensure that patients receive the best possible care and advice for managing their symptoms and preventing the spread of the disease.
Management of Dengue Fever

1. Triage of Suspected Dengue Patients
- Assess Severity: Determine whether the patient has mild, moderate, or severe dengue based on clinical signs and symptoms.
- Identify Warning Signs: Be vigilant for warning signs such as persistent vomiting, abdominal pain, mucosal bleeding, lethargy, and restlessness.
2. Approach to Clinical Management
- Fluid Balance: Monitor fluid intake and output closely. Measure ins and outs at least every shift and vital signs at least every 4 hours.
- Hematocrit Levels: Measure hematocrits every 6–12 hours during the critical period (24–48 hours after defervescence).
- Early Shock Recognition: Identify early shock (compensated or normotensive shock) characterized by narrowing pulse pressure, increased heart rate, and delayed capillary refill.
- Fluid Overload: Be cautious about fluid overload. Use only the minimum amount of intravenous (IV) fluid necessary to maintain perfusion.
- Colloids for Refractory Shock: If patients do not respond to isotonic saline, consider administering colloids (e.g., albumin) for refractory shock.
- PRBCs or Whole Blood for Bleeding: Transfuse packed red blood cells (PRBCs) or whole blood if there is clinically significant bleeding.
3. Management of Severe Hemorrhage
- Immediate Transfusion: If hematocrit drops with unstable vital signs or significant bleeding occurs, transfuse blood promptly.
4. Management of Convalescence Phase
- Monitor Recovery: Observe patients during the convalescence phase.
- Prognosis: Educate patients and their families about the expected course of recovery.
5. Management of Complications
- Address complications promptly, including dengue hemorrhagic fever, thrombocytopenia, and organ dysfunction.
6. Special Considerations
- Dengue in High-Risk Groups: Manage dengue in patients with co-morbidities and co-infections.
- Dengue and COVID-19 Co-Infection: Understand the case classification and management of co-infection.
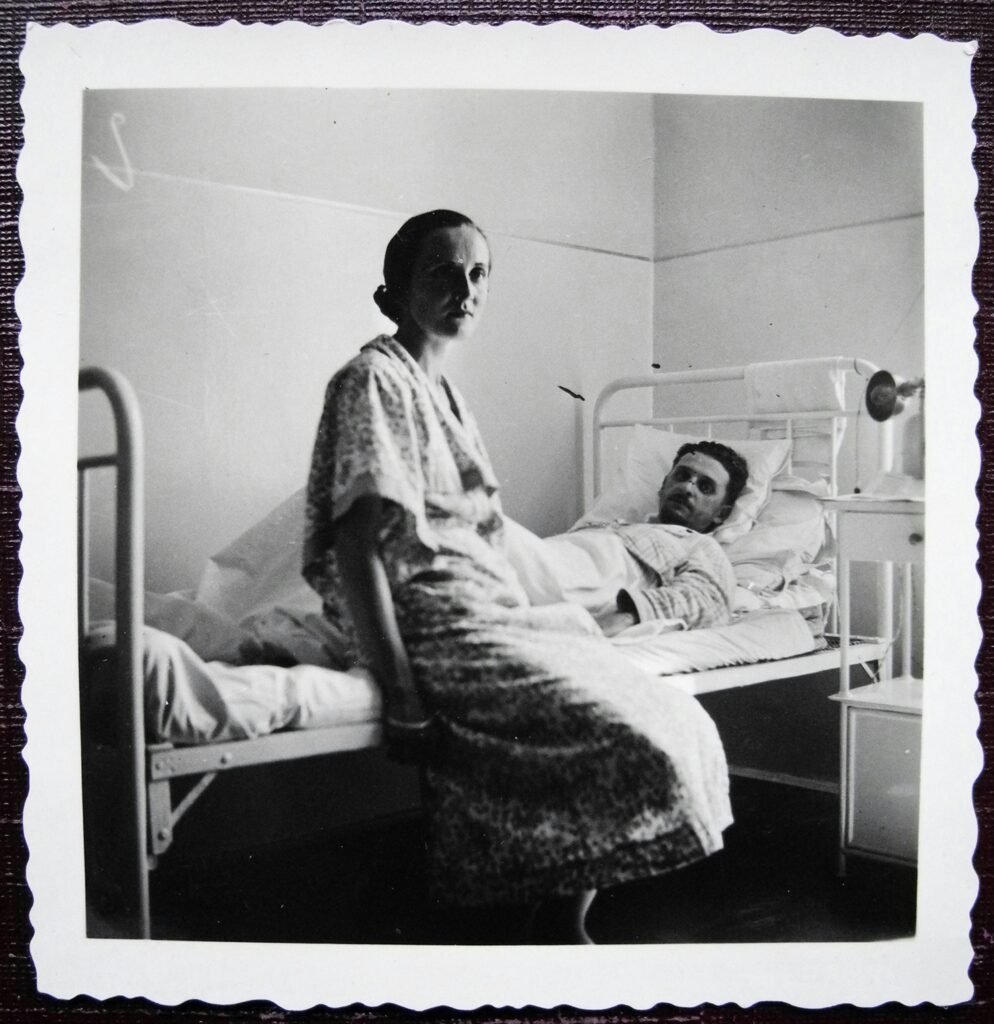
7. Nursing Care in Admitted Cases
- Provide supportive care, monitor vital signs, and ensure proper hydration.
8. Criteria for Admission
- Admit dengue disease patients to the hospital based on specific criteria.
9. Discharge from Hospital
- Discharge patients when stable and adequately recovered.
Remember that dengue management primarily focuses on supportive care, monitoring, and addressing complications. As a healthcare professional, your vigilance and timely interventions can significantly impact patient outcomes.
Complications of Dengue Fever
- Dengue Hemorrhagic Fever (DHF):
- DHF is a severe form of dengue characterized by increased bleeding from various body parts.
- Key features include:
- Decreased platelet count (thrombocytopenia).
- Leakage of blood plasma from blood vessels (vascular permeability).
- DHF can lead to shock and organ failure if not promptly managed.
- Dengue Shock Syndrome (DSS):
- DSS occurs when blood pressure falls significantly (below 20 mmHg) due to severe plasma leakage.
- Peripheral vascular collapse accompanies this condition.
- Early recognition and aggressive fluid management are crucial to prevent fatal outcomes.
- Episodes of Reduced Consciousness:
- Dengue virus can infect the brain, leading to inflammation and altered consciousness.
- Patients may experience confusion, drowsiness, or even coma.
- Risk for Pregnant Women:
- Pregnant women with dengue are at an increased risk of miscarriage.
- Dengue disease during pregnancy can also result in low birth weight and premature birth.
- Fatigue and Memory Impairment:
- After recovering from acute dengue, some individuals may experience fatigue, somnolence, and difficulty concentrating.
- Memory impairment can also occur.
Prevention of Dengue Fever
- Dengue Fever Vaccine:
- Consider getting vaccinated against dengue if available in your region.
- Mosquito Avoidance:
- Drain stagnant water to prevent mosquito breeding.
- Apply oil or insecticides to open water sources.
- Sleep under mosquito nets.
- Use insect repellents.
- Wear protective clothing that covers the whole body.
Remember, early diagnosis, proper management, and preventive measures play a crucial role in minimizing the impact of dengue fever. If you experience symptoms after traveling to an endemic area, seek medical attention promptly. Stay informed and protect yourself from mosquito bites! 🌿
The latest advancements in dengue vaccination are promising and offer new hope for the prevention of this disease. Here’s what you need to know about the current state of dengue vaccines:
QDENGA® (Dengue Tetravalent Vaccine [Live, Attenuated], TAK-003)
- Approval: QDENGA® has been approved for use in the European Union for individuals four years of age and older.
- Usage: It is the only dengue vaccine approved in the EU for use in individuals regardless of previous dengue exposure.
- Significance: This approval is a significant milestone in the global fight against dengue, offering a new tool for healthcare providers in dengue prevention.
Dengvaxia® (CYD-TDV)
- Availability: Dengvaxia® is available for use in areas with risk of dengue in the United States2.
- Recommendation: The CDC recommends dengue vaccination with Dengvaxia® for children 9 through 16 years old, but only when they have been previously infected with dengue and live in areas where dengue is common2.
- Consideration: Healthcare providers should check for evidence of a laboratory-confirmed previous dengue infection before vaccination due to increased risk for severe dengue disease and hospitalization if vaccinated children get dengue without prior infection2.
General Information
- Vaccination Strategy: Effective dengue prevention requires a multi-faceted approach, including vaccination as a key component.
- Travel Considerations: With the ease of global travel, vaccination is also important for individuals traveling to dengue-endemic regions.
It’s important to note that while these vaccines represent a significant step forward, they are not universally recommended for all individuals. Vaccination decisions should be made in consultation with healthcare professionals, taking into account individual risk factors and local dengue epidemiology.
For more detailed information on the latest dengue vaccines, consult the European Medicines Agency, the Centers for Disease Control and Prevention, and other reputable health organizations12. If you have further questions or need assistance with other health-related topics, feel free to ask! 🌿
The latest advancements in dengue vaccination are promising and offer new hope for the prevention of this disease. Here’s what you need to know about the current state of dengue vaccines:
QDENGA® (Dengue Tetravalent Vaccine [Live, Attenuated], TAK-003)
- Approval: QDENGA® has been approved for use in the European Union for individuals four years of age and older1.
- Usage: It is the only dengue vaccine approved in the EU for use in individuals regardless of previous dengue exposure1.
- Significance: This approval is a significant milestone in the global fight against dengue, offering a new tool for healthcare providers in dengue prevention1.
Dengvaxia® (CYD-TDV)
- Availability: Dengvaxia® is available for use in areas with risk of dengue in the United States.
- Recommendation: The CDC recommends dengue vaccination with Dengvaxia® for children 9 through 16 years old, but only when they have been previously infected with dengue and live in areas where dengue is common.
- Consideration: Healthcare providers should check for evidence of a laboratory-confirmed previous dengue infection before vaccination due to increased risk for severe dengue disease and hospitalization if vaccinated children get dengue without prior infection.
General Information
- Vaccination Strategy: Effective dengue prevention requires a multi-faceted approach, including vaccination as a key component.
- Travel Considerations: With the ease of global travel, vaccination is also important for individuals traveling to dengue-endemic regions.
It’s important to note that while these vaccines represent a significant step forward, they are not universally recommended for all individuals. Vaccination decisions should be made in consultation with healthcare professionals, taking into account individual risk factors and local dengue epidemiology.
Conclusion
In conclusion, dengue disease is a formidable global health challenge that affects millions each year. Understanding the signs and symptoms—such as sudden high fever, severe headaches, and joint pains—is crucial for early detection and treatment. While the diagnosis of dengue can be complex, modern medical tests provide accurate identification, enabling timely management to alleviate symptoms and prevent severe complications.
Management of dengue disease primarily involves supportive care, with vigilant monitoring for any signs of progression to more severe forms of the disease. Complications like dengue haemorrhagic fever and dengue shock syndrome are serious but can be managed effectively with prompt medical attention.
Prevention remains our best defense against dengue. Simple measures like mosquito control, using repellents, and wearing protective clothing can significantly reduce the risk of infection. Moreover, the advent of vaccines like QDENGA® and Dengvaxia® offers additional layers of protection for those at risk, particularly in endemic regions.
As we continue to combat dengue disease, it’s important for everyone to stay informed and proactive. Whether you’re a healthcare professional, a traveler to tropical regions, or a resident in a dengue-prone area, your awareness and actions can make a difference. By arming ourselves with knowledge and taking preventive steps, we can work together to lessen the impact of this disease on individuals and communities worldwide.
Remember, if you suspect you or someone you know may have dengue disease, seek medical advice promptly. Early intervention can lead to a better outcome and a quicker return to health. Stay safe, stay informed, and let’s keep fighting the bite!
If you have further questions or need assistance with other health-related topics, feel free to ask! 🌿


I really appreciate how thorough and clear this post was. Thanks!
Thanks for sharing. I read many of your blog posts, cool, your blog is very good.