
Table of Contents
Introduction
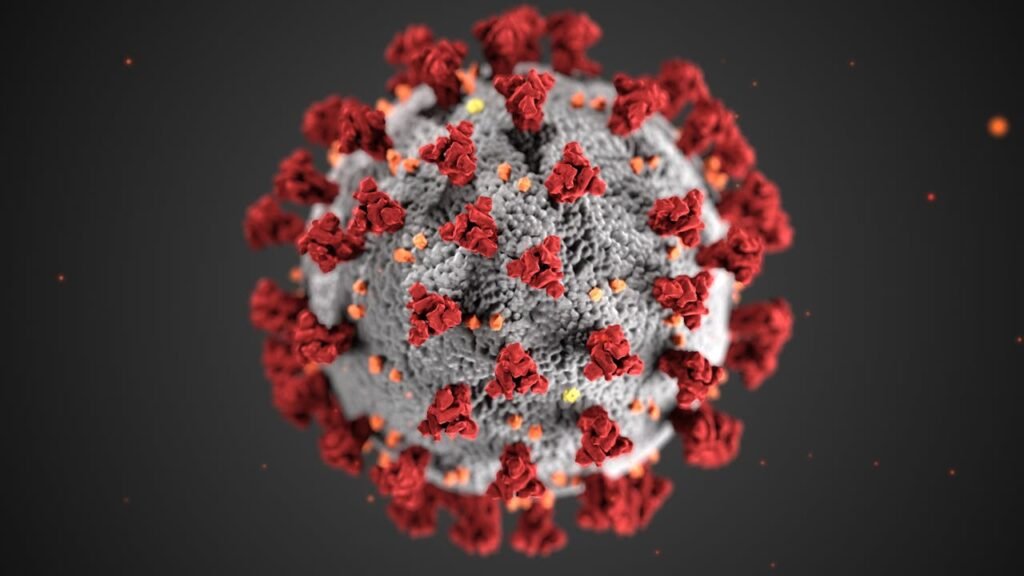
In recent months, the world has witnessed a concerning rise in monkeypox cases, sparking fear and confusion among the public. As a healthcare professional, it’s crucial to provide accurate and timely information to help people understand this emerging threat. Monkeypox, a rare but potentially serious viral illness, has been making headlines due to its rapid spread and the severity of its symptoms.
This article aims to shed light on monkeypox by exploring its symptoms, modes of transmission, prevention strategies, and treatment options. By raising awareness and dispelling myths, we can empower individuals to take proactive steps in protecting themselves and their communities. Let’s delve into the essential facts about monkeypox and learn how to stay safe during this outbreak.
What is Monkeypox?
Monkeypox is a viral disease caused by the monkeypox virus, a member of the Orthopoxvirus genus in the Poxviridae family1. This virus is closely related to the viruses that cause smallpox and cowpox1. Despite its name, the primary animal reservoirs for the monkeypox virus are not monkeys but small mammals like squirrels and rodents2.
First identified in 1958 in laboratory monkeys in Denmark, the first human case was recorded in 1970 in the Democratic Republic of the Congo1. Monkeypox is a zoonotic disease, meaning it can be transmitted from animals to humans and vice versa3. The disease presents with symptoms similar to smallpox but is generally less severe4.
Common symptoms of monkeypox include fever, headache, muscle aches, back pain, low energy, and swollen lymph nodes, followed by a rash that can last for 2-4 weeks1. The rash typically starts on the face and then spreads to other parts of the body, including the genitals3. The lesions go through several stages before eventually forming scabs and falling off5.
Understanding monkeypox is crucial for effective prevention and control, especially given its potential to cause significant outbreaks. By staying informed about the nature of the virus and its transmission, we can better protect ourselves and our communities.
Differences Between Monkeypox and Other Poxviruses

Monkeypox is part of the Orthopoxvirus genus, which includes several other notable viruses such as smallpox (variola virus), cowpox, and vaccinia virus. While these viruses share some similarities, there are key differences that distinguish monkeypox from the others.
1. Causative Agent
- Monkeypox: Caused by the monkeypox virus (MPXV), which has two distinct clades: Clade I (Central African) and Clade II (West African)1.
- Smallpox: Caused by the variola virus, which has been eradicated globally since 19802.
- Cowpox: Caused by the cowpox virus, primarily affecting rodents and occasionally transmitted to humans3.
- Vaccinia: Used in the smallpox vaccine, the vaccinia virus is less pathogenic and is used for immunization purposes4.
2. Transmission
- Monkeypox: Transmitted through direct contact with infected animals or humans, and through respiratory droplets1.
- Smallpox: Spread primarily through respiratory droplets and direct contact with infected bodily fluids or contaminated objects2.
- Cowpox: Typically transmitted from animals (especially cats and rodents) to humans through direct contact3.
- Vaccinia: Not naturally occurring; transmission is primarily through vaccination4.
3. Symptoms
- Monkeypox: Symptoms include fever, headache, muscle aches, back pain, swollen lymph nodes, and a characteristic rash that progresses through several stages1.
- Smallpox: Characterized by high fever, fatigue, and a distinctive rash that develops into pustules and scabs2.
- Cowpox: Causes localized skin lesions, often on the hands or face, and mild systemic symptoms3.
- Vaccinia: Generally mild symptoms, including localized skin reactions at the site of vaccination4.
4. Severity and Mortality
- Monkeypox: Generally less severe than smallpox, with a mortality rate varying between 1-10% depending on the clade1.
- Smallpox: Highly severe with a historical mortality rate of about 30%2.
- Cowpox: Usually mild and self-limiting in humans3.
- Vaccinia: Rarely causes severe illness, primarily used for vaccination4.
5. Geographical Distribution
- Monkeypox: Endemic in Central and West Africa, with occasional outbreaks in other regions1.
- Smallpox: Eradicated worldwide, with no natural cases since 19802.
- Cowpox: Found in Europe and parts of Russia3.
- Vaccinia: Used globally in the smallpox vaccination program4.
Understanding these differences is crucial for effective diagnosis, treatment, and prevention of these diseases. Each virus has unique characteristics that influence its spread, impact, and the strategies needed to control it.
Symptoms of Monkeypox
Early Signs and Symptoms
Monkeypox symptoms typically begin 5 to 13 days after exposure to the virus, but the incubation period can range from 5 to 21 days1. The early signs are often flu-like and can include:
- Fever: Often the first symptom to appear.
- Headache: Persistent and severe.
- Muscle Aches: Generalized body pain.
- Back Pain: Commonly reported.
- Fatigue: Extreme tiredness and lack of energy.
- Chills: Accompanied by fever.
- Swollen Lymph Nodes: A distinguishing feature from smallpox, occurring in the neck, armpits, or groin2.
Progression of the Disease
After the initial symptoms, a rash typically develops 1 to 3 days later3. The rash progresses through several stages:
- Macules: Flat, discolored lesions.
- Papules: Raised bumps.
- Vesicles: Fluid-filled blisters.
- Pustules: Pus-filled lesions.
- Scabs: Lesions that crust over and eventually fall off4.
The rash often starts on the face and then spreads to other parts of the body, including the palms of the hands, soles of the feet, and genital areas3. The number of lesions can vary from a few to several thousand1. The entire illness typically lasts 2 to 4 weeks4.
Severe Symptoms and Complications
While monkeypox is generally less severe than smallpox, it can still lead to significant complications, especially in vulnerable populations such as children, pregnant women, and immunocompromised individuals2. Severe symptoms and complications can include:
- Bronchopneumonia: A serious lung infection.
- Sepsis: A life-threatening response to infection.
- Encephalitis: Inflammation of the brain.
- Secondary Infections: Bacterial infections of the skin or other organs.
- Corneal Infection: Leading to vision loss3.
Understanding the symptoms and progression of monkeypox is crucial for early detection and effective management. Prompt medical attention can help mitigate severe complications and improve outcomes.
Transmission of Monkeypox
How Monkeypox Spreads
Human-to-Human Transmission Monkeypox can spread from person to person through several routes:
- Direct Contact: Touching the rash, scabs, or bodily fluids (like saliva) of an infected person1.
- Respiratory Droplets: Prolonged face-to-face contact can transmit the virus through respiratory secretions2.
- Contaminated Objects: Handling items such as clothing, bedding, or towels that have been in contact with an infected person2.
- Intimate Contact: Activities like kissing, hugging, or sexual contact can facilitate the spread of the virus2.
Animal-to-Human Transmission Monkeypox is a zoonotic disease, meaning it can be transmitted from animals to humans:
- Direct Contact with Infected Animals: Handling or being bitten or scratched by infected animals, such as rodents and primates1.
- Consumption of Infected Animal Meat: Eating undercooked meat from infected animals2.
- Contact with Animal Products: Handling animal products like fur or skin from infected animals1.
Risk Factors and Vulnerable Populations
Certain groups are at higher risk of contracting monkeypox and experiencing severe symptoms:
Risk Factors
- Close Contact: Individuals who have close physical contact with infected persons or animals are at higher risk1.
- Healthcare Workers: Due to their exposure to infected patients, healthcare workers are at increased risk3.
- Household Members: People living with someone who has monkeypox are more likely to contract the virus3.
- Travelers: Those traveling to regions where monkeypox is endemic, such as Central and West Africa, are at higher risk1.
Vulnerable Populations
- Children: More likely to experience severe symptoms and complications3.
- Pregnant Women: At risk of transmitting the virus to the fetus, which can lead to congenital monkeypox4.
- Immunocompromised Individuals: People with weakened immune systems are more susceptible to severe illness3.
Understanding how monkeypox spreads and identifying those at higher risk can help in implementing effective prevention and control measures. By staying informed and taking appropriate precautions, we can reduce the spread of this virus and protect vulnerable populations.
Prevention Strategies
Personal Hygiene and Protective Measures
Maintaining good personal hygiene and taking protective measures are essential to prevent the spread of monkeypox:
- Hand Hygiene: Wash your hands frequently with soap and water or use an alcohol-based hand sanitizer, especially after contact with potentially infected individuals or animals1.
- Avoid Close Contact: Refrain from close physical contact with people who have a rash resembling monkeypox. This includes avoiding kissing, hugging, or sexual contact1.
- Protective Clothing: Wear protective clothing, such as gloves and masks, when caring for someone with monkeypox or handling animals that could be infected1.
- Disinfection: Regularly clean and disinfect surfaces and objects that may be contaminated, such as bedding, towels, and clothing1.
- Isolation: Isolate infected individuals from healthy people to prevent the spread of the virus2.
Vaccination and Its Availability
Vaccination is a key tool in preventing monkeypox:
- JYNNEOS Vaccine: The JYNNEOS vaccine is a two-dose vaccine developed to protect against both monkeypox and smallpox. It is recommended for people at high risk of exposure, including healthcare workers and individuals who have had close contact with infected persons3.
- Availability: The JYNNEOS vaccine is available in many countries, including the United States, where it is covered by Medicare, Medicaid, and private insurance for eligible individuals3. Availability may vary, so it’s important to check with local health departments or healthcare providers for vaccine access4.
- Vaccination Schedule: The two doses of the JYNNEOS vaccine should be administered four weeks apart for optimal protection4.
Public Health Guidelines and Recommendations
Public health authorities provide guidelines to help control the spread of monkeypox:
- Isolation and Quarantine: Infected individuals should be isolated until all lesions have healed and a fresh layer of skin has formed. Close contacts may need to be quarantined and monitored for symptoms5.
- Reporting and Surveillance: Healthcare providers should report suspected cases to public health authorities to facilitate contact tracing and control measures6.
- Travel Advisories: Travelers to regions where monkeypox is endemic should avoid contact with animals that could carry the virus and follow local health guidelines5.
- Community Education: Public health campaigns should educate communities about monkeypox symptoms, transmission, and prevention strategies6.
By following these prevention strategies, individuals and communities can reduce the risk of monkeypox transmission and protect public health.
Diagnosis and Testing
How Monkeypox is Diagnosed
Diagnosing monkeypox involves a combination of clinical evaluation and laboratory testing. Healthcare providers start by assessing the patient’s symptoms, medical history, and potential exposure to the virus1. Key steps in the diagnosis include:
Clinical Evaluation:
Laboratory Testing:
- Sample Collection: Fluid from skin lesions, scabs, or respiratory secretions is collected using swabs2.
- Polymerase Chain Reaction (PCR): The primary method for confirming monkeypox. PCR tests detect the DNA of the monkeypox virus in the collected samples3.
- Serological Tests: These tests can detect antibodies against the monkeypox virus, indicating a past or recent infection4.
Available Testing Methods and Their Accuracy
Several testing methods are available to diagnose monkeypox, each with varying degrees of accuracy:
Polymerase Chain Reaction (PCR):
- Description: PCR is the gold standard for diagnosing monkeypox. It amplifies the viral DNA present in the sample, allowing for precise detection5.
- Accuracy: Highly accurate with a sensitivity and specificity close to 100% when performed correctly5.
- Turnaround Time: Results are typically available within 2-4 days5.
Genome Sequencing:
Serological Tests:
Isothermal Amplification Methods:
Electron Microscopy:
Accurate diagnosis of monkeypox is essential for effective treatment and containment of the virus. By utilizing these advanced testing methods, healthcare providers can ensure timely and precise identification of monkeypox cases.
Treatment Options
Current Treatment Protocols
Currently, there is no specific treatment approved exclusively for monkeypox (mpox) infections1. Most patients with intact immune systems and no severe skin conditions recover with supportive care and pain management1. However, for those with severe manifestations or at high risk (e.g., immunocompromised individuals), certain antiviral medications and supportive treatments are recommended1.
Supportive Care and Antiviral Medications
Supportive Care:
- Pain Management: Over-the-counter pain relievers like ibuprofen (Advil, Motrin) and acetaminophen (Tylenol) can help alleviate pain and reduce fever2.
- Hydration: Ensuring adequate fluid intake is crucial to prevent dehydration2.
- Skin Care: Keeping the rash clean and dry, and using gauze or bandages to cover lesions can help prevent secondary infections2.
Antiviral Medications:
- Tecovirimat (TPOXX): An antiviral medication available under an expanded access protocol. It has shown promise in treating monkeypox by inhibiting the virus’s ability to spread1.
- Brincidofovir and Cidofovir: These antivirals, originally developed for other viral infections, may also be used in severe cases of monkeypox3.
- Vaccinia Immune Globulin Intravenous (VIGIV): Used in certain severe cases, especially for patients with complications3.
Managing Symptoms at Home
For most people, monkeypox can be managed at home with the following measures24:
Isolation:
Symptom Relief:
- Pain and Fever: Use over-the-counter medications like ibuprofen or acetaminophen to manage pain and fever2.
- Rash Care: Keep the rash clean and dry. Avoid scratching or popping lesions to prevent spreading the virus and secondary infections2.
- Oral Lesions: Rinse with salt water or use prescribed mouthwashes to manage pain and keep the mouth clean2.
Hygiene and Disinfection:
Nutrition and Rest:
By following these treatment protocols and supportive care measures, most individuals can recover from monkeypox without severe complications. However, it’s important to seek medical advice if symptoms worsen or if you belong to a high-risk group.
Global Impact and Statistics
Recent Statistics on Monkeypox Cases Worldwide
As of August 2024, the global monkeypox outbreak has resulted in a total of 103,429 confirmed cases and 225 deaths across 121 countries1. The outbreak, which began in May 2022, has seen significant numbers of cases in various regions, with the highest concentrations in Europe and the Americas1. The World Health Organization (WHO) declared the outbreak a public health emergency of international concern due to its rapid spread and the severity of the disease2.
Impact on Different Regions and Populations
The impact of monkeypox has varied significantly across different regions and populations:
1. Europe and the Americas:
- Europe: The WHO European Region has reported the highest number of cases, accounting for approximately 86% of the global total3. Countries like the United Kingdom, Spain, and Germany have seen substantial outbreaks, primarily among men who have sex with men2.
- Americas: The Americas, particularly the United States and Brazil, have also experienced significant outbreaks, contributing to about 11% of the global cases3. Public health campaigns and vaccination efforts have been crucial in controlling the spread in these regions2.
2. Africa:
- Central and West Africa: Monkeypox is endemic in several Central and West African countries, including the Democratic Republic of the Congo and Nigeria4. These regions have faced ongoing challenges due to limited healthcare infrastructure and resources4.
- Impact on Vulnerable Populations: In Africa, children, pregnant women, and immunocompromised individuals are particularly vulnerable to severe outcomes from monkeypox5.
3. Other Regions:
- Eastern Mediterranean and Western Pacific: These regions have reported fewer cases, with less than 1% of the global total3. However, sporadic cases linked to travel or imported animals have been noted3.
4. Socioeconomic Impact:
- The outbreak has strained healthcare systems worldwide, particularly in regions with limited resources4. The economic impact includes increased healthcare costs and disruptions to daily life and travel5.
Understanding the global impact and statistics of monkeypox is essential for developing effective public health strategies and ensuring that resources are allocated to the most affected regions and populations.
Myths and Facts about Monkeypox
Common Misconceptions
Myth: Monkeypox was created in a lab.
- Fact: Monkeypox is a zoonotic disease, meaning it can be transmitted from animals to humans. It was first identified in 1958 in monkeys used for research, but it was not created in a lab1.
Myth: Monkeypox is a new disease.
- Fact: Monkeypox has been known since the 1970s when the first human case was recorded in the Democratic Republic of the Congo. It is not a new disease1.
Myth: You can get monkeypox from a swimming pool.
- Fact: Monkeypox does not spread through water. However, close physical contact with someone who has monkeypox lesions or using contaminated items like towels can transmit the virus1.
Myth: Only gay and bisexual men are at risk of catching monkeypox.
Myth: You can get monkeypox from public toilet seats or trying on clothes in stores.
- Fact: The virus can linger on surfaces, but transmission through casual contact like using a public toilet or trying on clothes is highly unlikely. Most cases result from prolonged skin-to-skin contact2.
Myth: Monkeypox spreads easily through the air like COVID-19.
- Fact: Monkeypox does not spread as easily through the air. It requires prolonged face-to-face contact or direct contact with bodily fluids, lesions, or contaminated materials2.
Evidence-Based Facts to Dispel Myths
Fact: Monkeypox is a zoonotic disease.
Fact: Monkeypox has been known for decades.
Fact: Monkeypox spreads through close contact.
Fact: Anyone can get monkeypox.
- The virus does not discriminate based on sexual orientation. Close physical contact with an infected person is the main risk factor2.
Fact: Surface transmission is rare.
- While the virus can survive on surfaces, the risk of transmission through casual contact with contaminated surfaces is low. Proper hygiene and disinfection can mitigate this risk2.
Fact: Airborne transmission is limited.
- Unlike COVID-19, monkeypox requires prolonged close contact for respiratory transmission. It is not known to linger in the air for extended periods2.
Conclusion
In summary, monkeypox is a zoonotic viral disease that has recently seen a significant rise in cases worldwide. Understanding its symptoms, modes of transmission, and prevention strategies is crucial for effective management and control. Early signs include fever, headache, and swollen lymph nodes, followed by a characteristic rash. The virus spreads through direct contact with infected individuals or animals, and certain populations, such as children and immunocompromised individuals, are more vulnerable to severe outcomes.
Prevention strategies include maintaining good personal hygiene, avoiding close contact with infected individuals, and following public health guidelines. Vaccination, particularly with the JYNNEOS vaccine, is a key tool in preventing monkeypox, especially for high-risk groups. Accurate diagnosis through PCR testing and supportive care, including antiviral medications, are essential for managing the disease.
Call to Action: Stay informed about monkeypox by following updates from reliable health organizations like the WHO and CDC. Practice good hygiene, avoid close contact with infected individuals, and seek medical advice if you experience symptoms. By taking these preventive measures, we can protect ourselves and our communities from the spread of monkeypox.
Frequently Asked Questions About Monkeypox
1. What is monkeypox?
Monkeypox is a viral disease caused by the monkeypox virus, which belongs to the Orthopoxvirus genus. It is similar to smallpox but generally less severe1.
2. How does monkeypox spread?
Monkeypox spreads through direct contact with the rash, scabs, or bodily fluids of an infected person. It can also spread through respiratory droplets during prolonged face-to-face contact and by touching contaminated objects1.
3. What are the symptoms of monkeypox?
Symptoms include fever, headache, muscle aches, back pain, swollen lymph nodes, chills, and exhaustion. A rash that progresses through several stages, including macules, papules, vesicles, pustules, and scabs, typically follows1.
4. How is monkeypox diagnosed?
Monkeypox is diagnosed through clinical evaluation and laboratory testing. PCR tests are the gold standard for confirming the presence of the monkeypox virus2.
5. Is there a vaccine for monkeypox?
Yes, the JYNNEOS vaccine is available and recommended for people at high risk of exposure, such as healthcare workers and individuals who have had close contact with infected persons2.
6. How can I prevent monkeypox?
Preventive measures include practicing good hand hygiene, avoiding close contact with infected individuals, using protective clothing, and getting vaccinated if you are at high risk1.
7. What should I do if I think I have monkeypox?
If you suspect you have monkeypox, isolate yourself from others and contact a healthcare provider for testing and guidance. Avoid close contact with others until you have been evaluated3.
8. How long do monkeypox symptoms last?
Monkeypox symptoms typically last 2 to 4 weeks. The rash goes through several stages before eventually forming scabs and falling off1.
9. Can monkeypox be treated?
There is no specific treatment for monkeypox, but supportive care and antiviral medications like Tecovirimat (TPOXX) can help manage symptoms and reduce the severity of the disease2.
10. Who is at higher risk of severe monkeypox?
Children, pregnant women, and immunocompromised individuals are at higher risk of severe outcomes from monkeypox1.

