Table of Contents
Introduction
Malaria, a life-threatening disease that has plagued humanity for centuries, remains a critical global health challenge. Despite significant advances in medical science, it continues to affect millions of people worldwide, particularly in tropical and subtropical regions. The World Health Organization (WHO) estimates that nearly half of the world’s population is at risk of malaria, with substantial morbidity and mortality rates reported annually.
This article aims to shed light on the complexities of malaria, from its transmission to the latest strategies in treatment and prevention. As we delve into the intricacies of this ancient disease, we will explore the causative agents, the life cycle of Plasmodium parasites, and the clinical manifestations that make malaria both a fascinating and formidable foe.
For healthcare professionals, understanding the nuances of malaria is crucial for effective diagnosis and management. This comprehensive overview serves as a reference point, offering insights into current treatment protocols, emerging research, and the ongoing efforts to eradicate this persistent threat to public health.
As we start this journey through the microscopic world of malaria, let us arm ourselves with knowledge and join forces in the fight against this pervasive disease. The battle may be long, but with continued vigilance and innovation, we can aspire to a future where malaria is no longer a common scourge but a conquered adversary.
Understanding Malaria
Malaria is an infectious disease that has been a significant public health concern for millennia. It is caused by the Plasmodium parasites, which are transmitted to humans through the bites of infected female Anopheles mosquitoes. Once in the human bloodstream, the parasites travel to the liver, where they mature and reproduce. After multiplying, they re-enter the bloodstream and infect red blood cells, leading to the clinical symptoms associated with the disease.
There are five species of Plasmodium that cause malaria in humans:
- Plasmodium falciparum: Responsible for the most severe form of the disease and prevalent in the African continent.
- Plasmodium vivax: Known for causing relapsing infections and predominantly found in Asia and Latin America.
- Plasmodium ovale: Similar to P. vivax, it is less common and can remain dormant in the liver for extended periods.
- Plasmodium malariae: Causes a chronic infection that can persist for years without symptoms.
- Plasmodium knowlesi: A zoonotic species that is found in Southeast Asia and can cause severe disease in humans.
The life cycle of the Plasmodium parasite is complex, involving both human and mosquito hosts. In humans, the cycle begins when an infected mosquito injects sporozoites into the bloodstream. These sporozoites then travel to the liver, where they invade hepatocytes and multiply. The resulting merozoites are released back into the bloodstream, where they infect red blood cells and multiply further, leading to the symptomatic phase of the disease.
Epidemiologically, malaria is most commonly found in tropical and subtropical areas where the climate is conducive to mosquito breeding. Regions such as sub-Saharan Africa, South Asia, and parts of South America bear the highest burden of the disease. Factors such as temperature, humidity, and rainfall patterns significantly influence the distribution and prevalence of malaria.
Understanding the epidemiology and life cycle of malaria is crucial for developing effective prevention and control strategies. It also aids healthcare professionals in anticipating and recognizing the patterns of infection, which is essential for timely diagnosis and treatment.
In the following sections, we will explore the transmission dynamics, clinical features, and the latest advancements in the management of malaria, providing a holistic view of the disease and its impact on global health.
Transmission and Risk Factors
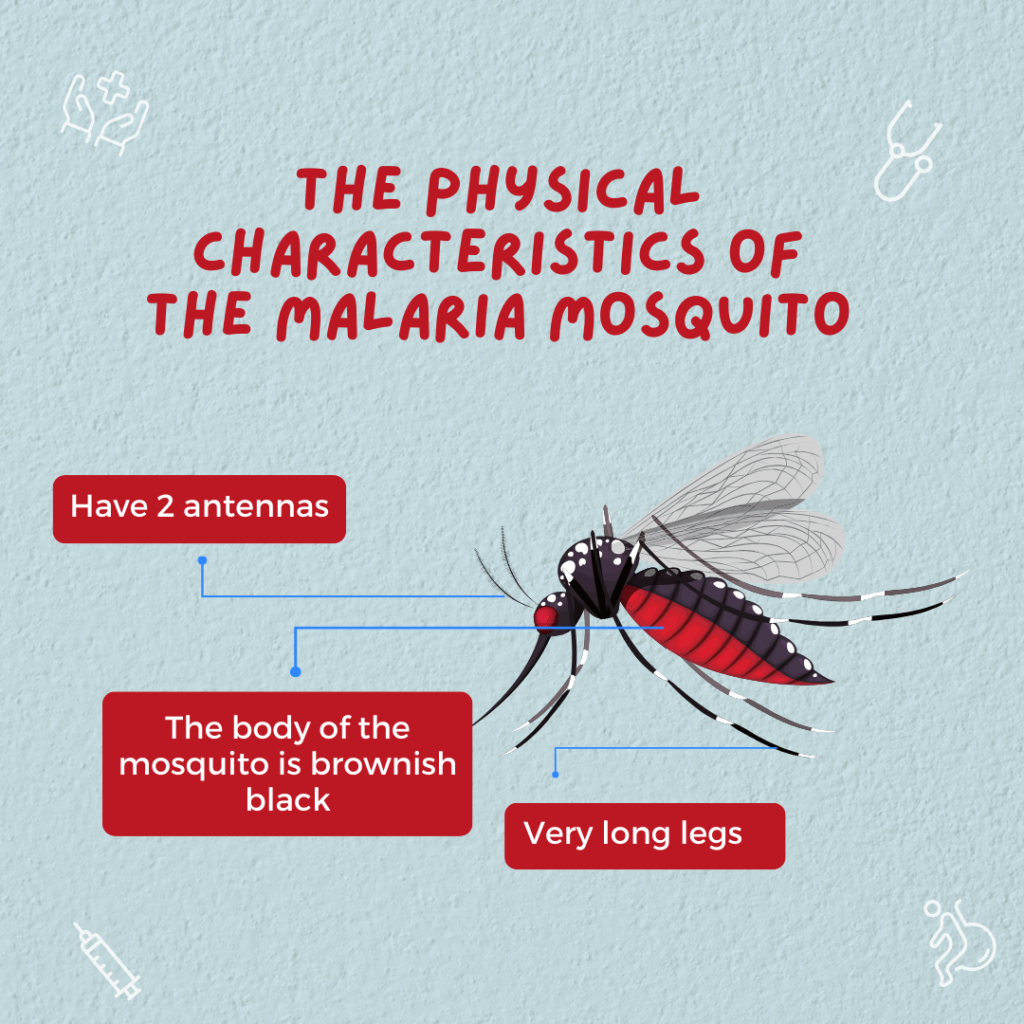
Malaria transmission occurs primarily through the bite of an infected female Anopheles mosquito. When a mosquito bites a person infected with malaria, it ingests the parasites along with the blood. Inside the mosquito, the parasites undergo a series of developmental changes, eventually reaching the salivary glands. When this mosquito bites another human, the parasites are transmitted and the cycle continues.
Modes of Transmission:
- Vector-borne transmission: The primary route, involving mosquitoes.
- Mother-to-child transmission (congenital malaria): Occurs when parasites are transmitted from mother to fetus during pregnancy.
- Blood transfusion: Can occur if infected blood is used.
- Organ transplant: If the donated organ comes from an infected individual.
- Shared needles/syringes: In areas with high rates of intravenous drug use.
Risk Factors:
- Geographical location: Proximity to mosquito breeding sites and endemic regions.
- Climate: Warm and humid climates with consistent rainfall are ideal for mosquito breeding.
- Socioeconomic status: Poorer regions often have less access to preventive measures and healthcare.
- Occupation: Outdoor night-time workers are at higher risk.
- Immunity: Individuals with weakened immune systems, such as young children and pregnant women, are more susceptible.
High-Risk Populations:
- Children under five years of age: They have not yet developed partial immunity to malaria.
- Pregnant women: Pregnancy reduces a woman’s immunity to malaria, making her more susceptible to infection and increasing the risk of severe disease.
- Travelers from non-endemic areas: Lack of immunity can lead to severe infections.
- Immigrants from endemic regions: May have decreased immunity after moving to areas with no malaria transmission.
Geographical Distribution: Malaria is prevalent in over 100 countries worldwide, with the highest transmission occurring in parts of Africa, Asia, and Latin America. Sub-Saharan Africa carries a disproportionately high share of the global malaria burden.
Climate Change and Its Impact: Climate change is altering the geographical distribution of malaria. Rising temperatures, changing precipitation patterns, and extreme weather events can expand the habitat of Anopheles mosquitoes, potentially introducing malaria to new regions and increasing the risk in areas where it is currently controlled.
Understanding the transmission dynamics and risk factors is essential for developing targeted interventions. By identifying and addressing the specific needs of high-risk populations and regions, we can reduce the incidence of malaria and move closer to the goal of eradication.
Clinical Features and Diagnosis
The clinical presentation of malaria is diverse, ranging from mild symptoms to severe disease and death. Early diagnosis and treatment are crucial in preventing complications and controlling the spread of the disease.
Clinical Features:
- Incubation Period: Typically ranges from 7 to 30 days for P. falciparum and can be longer for other species.
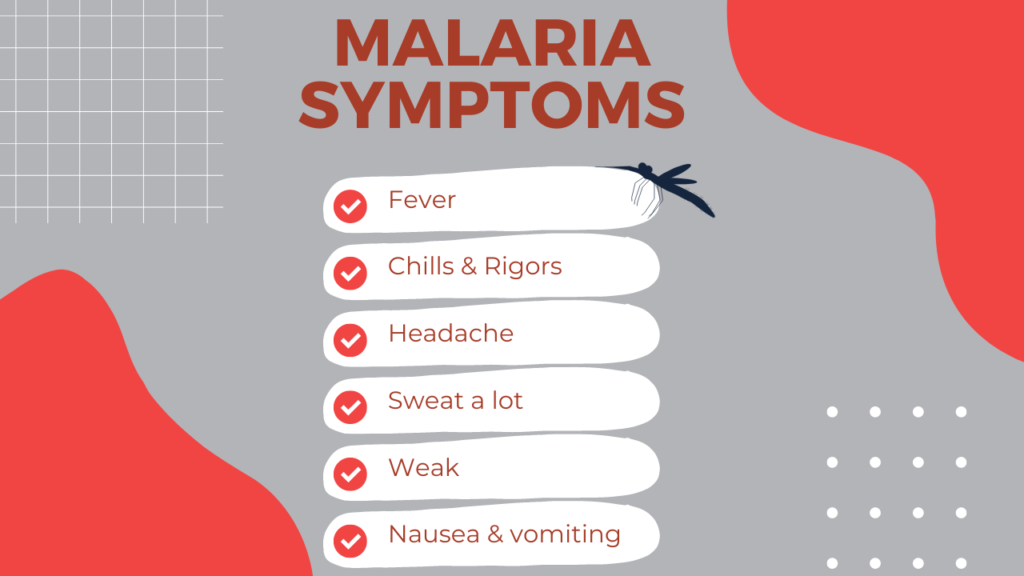
- Symptoms: Fever, chills, sweats, headaches, nausea, vomiting, body aches, and general malaise. In severe cases, it can progress to anemia, jaundice, seizures, mental confusion, kidney failure, and coma.
- Stages of Infection: The ‘cold stage’ characterized by shivering, followed by the ‘hot stage’ with fever and headaches, and then the ‘sweating stage’ with intense sweating and fatigue.
Diagnosis:
- Microscopic Examination: The gold standard for malaria diagnosis. Blood smears are examined under a microscope to detect the presence of Plasmodium parasites.
- Rapid Diagnostic Tests (RDTs): Provide results within 15-20 minutes and are useful in areas without laboratory facilities.
- Molecular Tests: Such as polymerase chain reaction (PCR), are highly sensitive and can detect low levels of parasites.
- Serology: Can detect antibodies against malaria but is not typically used for acute diagnosis.
Differential Diagnoses:
- Other conditions that present with fever and flu-like symptoms must be considered, such as dengue, typhoid fever, leptospirosis, and viral hemorrhagic fevers.
Challenges in Diagnosis:
- Asymptomatic Carriers: Individuals who carry the parasite without showing symptoms can still transmit the disease.
- Drug Resistance: Can lead to false negatives in RDTs if they are designed to detect specific antigens affected by resistance.
- Variability in Symptoms: The wide range of symptoms can lead to misdiagnosis, especially in areas where malaria is not endemic.
Accurate diagnosis is the cornerstone of effective malaria management. It enables healthcare providers to administer the correct treatment promptly, reducing the risk of severe disease and preventing further transmission. As we continue to improve diagnostic tools and techniques, our ability to combat malaria will only grow stronger.
Treatment Protocols
The treatment of malaria is a critical step in the management of the disease, with the primary goal being the complete elimination of the Plasmodium parasite from the patient’s blood. This section will outline the current treatment protocols for malaria, addressing drug resistance, and special considerations for complicated cases.
First-Line Treatments:
- Artemisinin-based Combination Therapies (ACTs): The WHO recommends ACTs as the first-line treatment for uncomplicated P. falciparum malaria. These therapies combine an artemisinin derivative with another antimalarial drug, enhancing efficacy and reducing the risk of resistance.
- Chloroquine: Effective against P. vivax, P. ovale, and P. malariae in areas without chloroquine resistance.
- Primaquine: Used for the radical cure of P. vivax and P. ovale to prevent relapse by targeting dormant liver stages.
Drug Resistance Issues:
- Resistance to Antimalarial Drugs: A growing concern, particularly with P. falciparum’s resistance to artemisinin and its derivatives in some regions.
- Monitoring and Surveillance: Essential for detecting and responding to resistance patterns.
- Combination Therapies: Recommended to delay the development of resistance.
Treatment for Complicated Malaria:
- Severe Malaria: Requires hospitalization and intravenous administration of antimalarial drugs, such as artesunate.
- Supportive Care: Management of complications like anemia, hypoglycemia, and renal failure is crucial.
Case Management in Pregnancy:
- Special Considerations: Pregnant women are more susceptible to malaria and its adverse outcomes, which can include maternal anemia, fetal loss, and low birth weight.
- Treatment Options: The choice of antimalarial drugs in pregnancy is limited due to potential teratogenic effects. ACTs are recommended in the second and third trimesters, while quinine plus clindamycin is preferred in the first trimester.
Pediatric Considerations:
- Dosage Adjustments: Children require weight-based dosing of antimalarial medications.
- Formulations: Pediatric formulations and dispersible tablets are available for younger children.
Effective treatment protocols are the cornerstone of malaria management. They not only cure the individual but also reduce the transmission of the parasite within the community. As resistance patterns evolve, so must our strategies for treatment, ensuring that we remain one step ahead in the fight against malaria.
Prevention Strategies
Preventing malaria is a multifaceted approach that involves reducing the risk of transmission and exposure to the Plasmodium parasite. Effective prevention not only protects individuals but also reduces the overall burden of the disease on communities and health systems. This section will discuss the various strategies employed to prevent malaria.
Vector Control Measures:
- Insecticide-Treated Mosquito Nets (ITNs): Widely distributed and used to protect people from mosquito bites during sleep.
- Indoor Residual Spraying (IRS): Application of insecticides on the interior walls of homes to kill mosquitoes.
- Larval Source Management (LSM): Control of mosquito larvae by environmental management and application of larvicides.
Personal Protective Measures:
- Repellents: Use of insect repellent on skin and clothing.
- Protective Clothing: Wearing long sleeves and pants, especially during peak mosquito biting hours.
- Environmental Modifications: Reducing standing water and improving sanitation to decrease mosquito breeding sites.
Prophylactic Medications:
- Chemoprophylaxis: Taking antimalarial drugs preventively, particularly for travelers to high-risk areas.
- Intermittent Preventive Treatment (IPT): Regular administration of antimalarial drugs to high-risk groups, such as pregnant women (IPTp) and infants (IPTi).
Vaccination Developments:
- RTS,S/AS01 (Mosquirix): The first malaria vaccine recommended by WHO for children in regions with moderate to high P. falciparum malaria transmission.
- Research on New Vaccines: Ongoing efforts to develop more effective vaccines with broader protection and longer-lasting immunity.
Community Engagement and Education:
- Awareness Campaigns: Educating communities about malaria prevention and control.
- Community-Based Interventions: Involving local populations in vector control activities.
Monitoring and Evaluation:
- Surveillance Systems: Tracking malaria cases to monitor the effectiveness of prevention strategies.
- Data Analysis: Using data to inform policy decisions and allocate resources effectively.
Prevention strategies are the cornerstone of malaria control and require the concerted efforts of governments, health organizations, communities, and individuals. By employing a combination of these methods, we can significantly reduce the incidence of malaria and move closer to the goal of elimination.
Public Health Policies and Programs
The fight against malaria is not only a clinical challenge but also a public health endeavor. Effective policies and programs are essential to reduce the incidence and impact of malaria on a population level. This section will discuss the role of public health policies and programs in malaria control and elimination.
National Malaria Control Programs (NMCPs):
- Strategic Planning: Development of comprehensive plans that address local malaria epidemiology and resources.
- Implementation: Execution of malaria control interventions such as ITNs, IRS, and case management.
- Collaboration: Working with local and international partners to maximize resources and expertise.
International Efforts and Collaboration:
- World Health Organization (WHO): Provides guidelines, technical support, and global malaria strategy.
- Global Fund to Fight AIDS, Tuberculosis and Malaria: Offers financial support for malaria control programs.
- Roll Back Malaria (RBM) Partnership: Aims to coordinate global action against malaria.
Role of Non-Governmental Organizations (NGOs):
- Advocacy: Raising awareness and funds for malaria control.
- Research and Development: Supporting studies on new tools and interventions.
- Community-Based Programs: Implementing grassroots initiatives to combat malaria.
Success Stories:
- Reduction in Malaria Cases: Some countries have achieved significant reductions in malaria cases and deaths through concerted efforts.
- Elimination: Several countries have been certified malaria-free by the WHO in recent years.
Challenges:
- Funding Gaps: Sufficient and sustained funding is crucial for maintaining and scaling up malaria control efforts.
- Political Will: Strong commitment from government leaders is necessary to prioritize malaria control.
- Health Systems Strengthening: Robust health systems are needed to deliver effective malaria interventions.
Future Directions in Malaria Control:
- Innovation: Developing new tools and strategies to overcome challenges such as drug resistance and changing mosquito behavior.
- Integration: Incorporating malaria control into broader health initiatives to improve overall health outcomes.
- Sustainability: Ensuring that malaria control efforts are sustainable in the long term.
Public health policies and programs play a pivotal role in the global fight against malaria. By combining strategic planning, international collaboration, and community engagement, we can continue to make strides towards reducing the burden of malaria and ultimately achieving elimination.
Research and Innovations

The battle against malaria is bolstered by continuous research and innovation, which aim to improve our understanding of the disease and develop new tools for its prevention, diagnosis, and treatment. This section will delve into the recent advancements in malaria research and the promising innovations on the horizon.
Recent Advancements in Malaria Research:
- Genetic Studies: Understanding the genetics of both the Plasmodium parasite and the Anopheles mosquito to develop targeted interventions.
- Drug Development: Discovery of new antimalarial compounds with novel mechanisms of action to combat drug resistance.
- Vector Control: Development of new insecticides and genetically modified mosquitoes to reduce transmission.
Novel Diagnostic Tools:
- Rapid Diagnostic Tests (RDTs): Enhancements in sensitivity and specificity, allowing for the detection of low-parasite-density infections.
- Mobile Health Technologies: Use of mobile devices and applications to facilitate remote diagnosis and surveillance.
Emerging Treatment Options:
- Single-Dose Therapies: Research into drugs that can cure malaria with a single dose, improving compliance and reducing the risk of resistance.
- Vaccine Research Updates: Progress in the development of more effective vaccines that offer broader protection and longer-lasting immunity.
Vaccine Research Updates:
- RTS,S/AS01 (Mosquirix): Further studies on the implementation and long-term efficacy of the first WHO-recommended malaria vaccine.
- Next-Generation Vaccines: Exploration of vaccines targeting different stages of the parasite’s life cycle or providing cross-species protection.
Operational Research:
- Implementation Science: Studies on the best ways to implement and scale up effective malaria interventions in different settings.
- Health Economics: Analysis of the cost-effectiveness of malaria control measures and their impact on health systems.
Collaborative Efforts:
- Global Partnerships: Strengthening international collaborations to share knowledge and resources.
- Community Participation: Engaging local communities in research projects to ensure interventions are culturally appropriate and sustainable.
Challenges and Opportunities:
- Funding for Research: Securing adequate and sustained investment in malaria research is critical.
- Translational Research: Bridging the gap between laboratory findings and practical applications in the field.
The landscape of malaria research and innovation is dynamic and promising. With each new discovery and technological advancement, we move closer to a world free of malaria. By fostering a robust research environment and encouraging collaborative efforts, we can accelerate progress and turn scientific insights into real-world solutions.
Educating Healthcare Professionals
The eradication of malaria requires not only effective treatment and prevention strategies but also a well-informed healthcare workforce. Education and training for healthcare professionals are vital to ensure that they are equipped with the latest knowledge and skills to manage and prevent malaria. This section will focus on the importance of education for healthcare providers and the resources available to them.
Training on Malaria Management:
- Continuing Medical Education (CME): Regular CME programs to update healthcare professionals on the latest in malaria diagnosis, treatment, and prevention.
- Workshops and Seminars: Hands-on training sessions to enhance clinical skills and knowledge.
- Online Courses and Webinars: Accessible platforms for learning and staying informed about global malaria trends and research.
Importance of Continuous Medical Education:
- Keeping Up-to-Date: The malaria landscape is constantly changing with new research, drug resistance patterns, and vector control strategies.
- Clinical Competence: Ensuring that healthcare providers can competently manage both uncomplicated and severe cases of malaria.
- Public Health Impact: Educated healthcare professionals play a crucial role in reducing the burden of malaria through effective case management and public health initiatives.
Resources for Healthcare Providers:
- Guidelines and Protocols: Distribution of standardized treatment guidelines from reputable organizations like the WHO.
- Mobile Health Apps: Tools that provide quick access to information and decision support at the point of care.
- Professional Networks: Forums for healthcare providers to share experiences, discuss cases, and collaborate on malaria-related issues.
Challenges in Education:
- Resource Limitations: In some regions, there may be a lack of access to educational resources and training opportunities.
- Knowledge Translation: Bridging the gap between knowledge acquisition and practical application in diverse healthcare settings.
Future Directions:
- Simulation-Based Training: Using technology to simulate real-life scenarios for training purposes.
- Interdisciplinary Education: Encouraging collaboration between different healthcare disciplines to provide comprehensive malaria care.
- Research Opportunities: Involving healthcare professionals in research to foster a deeper understanding of malaria and contribute to scientific advancements.
By prioritizing the education of healthcare professionals, we can ensure a robust response to malaria. Continuous learning and professional development are key to maintaining high standards of care and adapting to the evolving challenges posed by this disease.
Conclusion
As we conclude this comprehensive exploration of malaria, it is clear that the disease remains a formidable challenge to global health. Despite the significant strides made in reducing its prevalence and impact, malaria continues to claim lives and strain healthcare systems, particularly in resource-limited settings.
Throughout this article, we have traversed the intricate landscape of malaria, from its transmission and clinical features to the innovative research and public health efforts aimed at its eradication. We have seen the importance of robust treatment protocols, the critical role of prevention strategies, and the value of continuous education for healthcare professionals.
The fight against malaria is a testament to the power of collective action. It requires the collaboration of governments, health organizations, communities, and individuals to implement effective interventions and sustain progress. As we move forward, it is imperative that we maintain the momentum gained through research and innovation, adapt to the evolving challenges of drug resistance and climate change, and continue to invest in the education and empowerment of those on the front lines.
In the spirit of shared responsibility, this article serves as a call to action for all stakeholders to renew their commitment to the fight against malaria. By harnessing the tools and knowledge at our disposal, we can envision a future where malaria is no longer a common threat but a distant memory. The road ahead may be long, but with perseverance and dedication, we can achieve a malaria-free world.
How can readers contribute to global efforts against malaria?
Stay Informed and Raise Awareness:
- Educate yourself about malaria, its impact, and the ongoing efforts to combat it.
- Share accurate information and educate others in your community.
Support Malaria Control Programs:
- Donate to reputable organizations that are working to prevent and treat malaria.
- Participate in fundraising events or campaigns that benefit malaria research and control efforts.
Advocate for Policy Change:
- Encourage political leaders and policymakers to prioritize malaria control and allocate necessary resources.
- Support policies that promote health equity and access to malaria prevention and treatment services.
Volunteer:
- Get involved with local or international health organizations that focus on malaria.
- Volunteer in community-based programs that aim to educate and implement prevention measures.
Promote Prevention Measures:
- Support the distribution of insecticide-treated mosquito nets and other preventive tools.
- Advocate for environmental management to reduce mosquito breeding sites.
Engage in Research and Innovation:
- Support research initiatives by participating in studies or providing financial backing.
- Stay updated on new developments, such as vaccines and novel treatments.
Practice Responsible Travel:
- If traveling to malaria-endemic areas, take prophylactic medications and use personal protective measures to prevent mosquito bites.
- Upon return, continue to monitor your health and seek medical attention if you experience symptoms of malaria.
Frequently Asked Questions (FAQs)
1. What is malaria? Malaria is a life-threatening disease caused by parasites that are transmitted to people through the bites of infected female Anopheles mosquitoes.
2. How is malaria transmitted? The primary mode of transmission is through the bite of an infected Anopheles mosquito. It can also be transmitted from a mother to her unborn child, through blood transfusions, and by sharing needles.
3. Who is at risk of contracting malaria? People living in or traveling to malaria-endemic areas, particularly in sub-Saharan Africa, South Asia, and parts of South America, are at risk. Young children, pregnant women, and travelers with little or no immunity are particularly vulnerable.
4. What are the symptoms of malaria? Symptoms include fever, chills, headache, sweats, fatigue, nausea, and vomiting. Severe cases can lead to anemia, jaundice, seizures, and coma.
5. How is malaria diagnosed? Malaria is diagnosed using blood tests to look for the presence of the parasite. The most common tests are microscopic examination of blood smears and rapid diagnostic tests (RDTs).
6. Is malaria treatable? Yes, malaria is treatable with antimalarial medications. The specific treatment depends on the type of parasite, the severity of the symptoms, and the patient’s overall health.
7. Can malaria be prevented? Preventive measures include using insecticide-treated mosquito nets, indoor residual spraying, taking antimalarial drugs (prophylaxis), and wearing protective clothing.
8. Is there a vaccine for malaria? Yes, the RTS,S/AS01 (Mosquirix) vaccine is recommended by the WHO for children in regions with moderate to high P. falciparum malaria transmission.
9. What is the difference between malaria elimination and eradication? Malaria elimination is the interruption of local transmission of a specified malaria parasite species in a defined geographic area. Eradication means the permanent reduction to zero of the worldwide incidence of malaria infection caused by all species of human malaria parasites.
10. How can I contribute to the fight against malaria? You can contribute by staying informed, donating to malaria control programs, advocating for policy change, volunteering, promoting prevention measures, and practicing responsible travel.

